Introduction: Medicaid Qualification: A Lifeline or a Labyrinth?
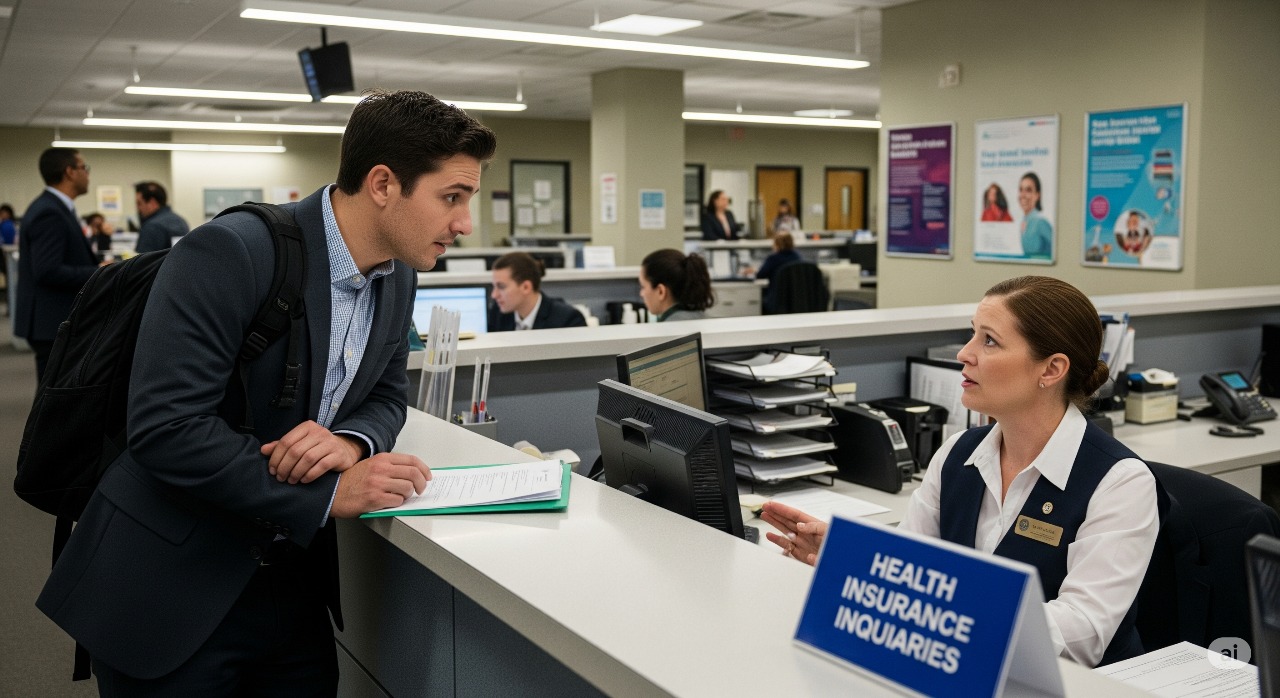
Medicaid is often touted as a vital safety net—the go-to insurance program for low-income Americans needing healthcare access. Yet, despite its importance, qualifying for Medicaid remains a complicated process that many find confusing, frustrating, or even discouraging. The phrase “how to qualify for Medicaid insurance in the USA” is not just a simple query; it reflects thousands of stories of struggle navigating a patchwork system.
This blog exposes the realities behind Medicaid eligibility. We critically examine eligibility criteria, the labyrinthine application process, and ongoing challenges that limit access. For Americans who need Medicaid most, understanding these barriers can empower better navigation and advocacy.
What Is Medicaid and Why Does Qualification Matter?
Medicaid is a joint federal and state program providing health coverage to eligible low-income adults, children, pregnant women, the disabled, and seniors. Unlike Medicare, which generally serves adults over 65 or with certain disabilities regardless of income, Medicaid’s crux is means-testing and need.
Why Qualifying Matters:
- Medicaid often covers doctor visits, hospital care, mental health, prescription drugs, and long-term care services unaffordable for many without insurance.
- Access to Medicaid can mean life-saving treatments, preventive care, and financial security versus catastrophic medical bills.
- Yet, many low-income Americans remain uninsured due to complex eligibility rules or bureaucratic obstacles.
Eligibility Criteria: Who Qualifies for Medicaid?
Income Limits Vary Widely
Medicaid eligibility heavily depends on household income relative to the federal poverty level (FPL). However, states set their own thresholds. In Medicaid expansion states, adults earning up to 138% of FPL are eligible, while in non-expansion states, eligibility remains far narrower.
Categorical Eligibility
Besides income, qualification depends on age, disability status, pregnancy, and family composition. Categories include:
- Pregnant women
- Children under certain ages
- Seniors with low income
- People with disabilities
- Parents or caretakers with dependent children (subject to state rules)
Asset and Residency Requirements
Some states apply asset tests, limiting total allowed savings. Residency and citizenship or immigration status are also factored, with exclusions or additional hurdles for some groups.
The Application Process: Why Is It So Complicated?
Applying for Medicaid can be daunting:
- Different Application Channels: States vary between online portals, in-person offices, phone, or mail applications.
- Documentation Overload: Proof of income, residency, disability, and more is required, often causing delays or denials due to missing paperwork.
- Waiting Periods and Retroactive Coverage: New applicants may face waiting times. Retroactive coverage exists but can be difficult to navigate.
- Renewal Hassles: Recertification is necessary, but notices get lost or misunderstood, causing coverage gaps.
Real-World Challenges and Systemic Failures
1. Geographic Inconsistency
States’ discretion leads to wildly uneven eligibility, coverage, and application support, creating a “postcode lottery” of access.
2. Administrative Burdens
Bureaucratic hurdles deter many qualified individuals, especially those with limited literacy, language skills, or disability.
3. Stigma and Lack of Awareness
Fear of public assistance stigma and lack of clear information prevent many from applying or completing applications.
4. Underfunding and Limited Outreach
Resource shortages mean states often cannot proactively assist applicants or streamline processes.

Timeline: Navigating Medicaid Qualification
- Pre-Application: Gather documents, and research state rules.
- Application Submission: Submit via chosen method with required paperwork.
- Initial Review: The State agency evaluates income and eligibility.
- Follow-Up Requests: Respond promptly to requests for additional info.
- Approval or Denial: Receive decision; denials may lead to appeals.
- Coverage Begins: Access benefits, subject to ongoing renewal requirements.
Tips for Successfully Qualifying for Medicaid
- Research Your State’s Specific Rules: Eligibility and application processes vary.
- Prepare Complete Documentation: Includes income statements, residency proof, IDs, and medical records if applicable.
- Seek Help: Nonprofits, navigators, and legal aid groups provide invaluable assistance.
- Be Prompt and Persistent: Timely responses to information requests speed approval.
- Appeal Denials: Don’t assume rejection is final; many can be overturned.
Conclusion:
Medicaid remains a cornerstone for health access in America. Yet, qualifying is anything but easy. The complex, patchwork system, fraught with inconsistent state rules, laborious applications, and limited resources, erects barriers many eligible individuals must overcome.
Awareness, preparation, and determination prove critical in conquering the process. Meanwhile, systemic reforms to simplify applications, harmonize eligibility, and increase outreach are urgently needed.
For millions relying on Medicaid, the difference between health security and vulnerability too often hinges on navigating the labyrinth. Together, consumers, advocates, and policymakers must forge a path to make Medicaid truly accessible.